“Don’t make me laugh until I can cross my legs…” “I gave up running because it was too embarrassing to have to wear pads…” If you can relate, then you are not alone. Over 50% of adult women in the United States experience urinary incontinence, which is loss of bladder control or leaking urine. Men suffer from this as well, with 11-34% prevalence reported in various studies, and more common with advancing age.
Normal Function
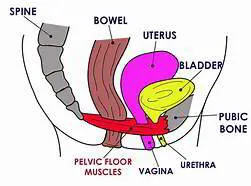
In order to understand why urinary incontinence occurs, you need to know what is involved in normal function. Urine is made by the kidneys and stored in the bladder. The bladder has muscles that tighten when you need to urinate. When the bladder muscles tighten, urine is forced out of your bladder through a tube called the urethra. At the same time, sphincter muscles around the urethra relax to let the urine out of your body. Pelvic floor muscles contract at the same time and assist the bladder in emptying urine and also support the urethra position.
Urinary Incontinence
The pelvic floor muscles that support the bladder, urethra, uterus, and bowels may become weaker or damaged with certain health conditions and with aging. When the muscles that support the urinary tract are weak, the muscles in the urinary tract must work harder to hold urine until you are ready to urinate. This extra stress or pressure on the bladder and urethra can cause urinary incontinence or leakage.
- Stress incontinence. This is the most common type of incontinence. Stress incontinence can happen when weak pelvic floor muscles put pressure on the bladder and urethra by making them work harder. Everyday actions that use the pelvic floor muscles, such as coughing, sneezing, or laughing, can cause you to leak urine. Sudden movements and physical activity can also cause you to leak urine. This is more common in women.
- Urge incontinence. Urine leakage usually happens after a strong, sudden urge to urinate and before you can get to a bathroom. Urge incontinence is sometimes called “overactive bladder.” This is more common in older men.
- Mixed incontinence. Urinary incontinence with components of both stress and urge incontinence.
Causes of Urinary Incontinence
In women, the most common causes of urinary incontinence include pregnancy, vaginal childbirth as well as previous hysterectomy. With aging and onset of menopause, even women without pregnancy or surgical history can suffer from urinary incontinence.
In men, the most common cause urge incontinence is enlarged prostate which constricts the urethra, causing back up of urine in the bladder. Aging changes but also surgery for enlarged prostate or prostate cancer result in damage and weakening of the pelvic floor muscles and cause stress incontinence.
Other causes of urinary incontinence in both women and men include:
- Having excess weight puts pressure on the bladder, which can weaken the muscles over time.
- Chronic constipation, or straining to have a bowel movement, can put stress or pressure on the bladder and pelvic floor muscles. This weakens the muscles and can cause urinary incontinence or leaking.
- Damaged nerves may send signals to the bladder at the wrong time or not at all. Health problems like diabetes and Parkinson’s disease or multiple sclerosis can cause nerve damage in the bladder, urethra, or pelvic floor muscles.
Sometimes urinary incontinence lasts only for a short time and happens because of other reasons, including:
- Urinary incontinence may be a side effect of medicines such as diuretics, sedatives, muscle relaxants and often goes away when you stop taking the medicine.
- Drinks with caffeine can cause the bladder to fill quickly, which can cause you to leak urine. Studies suggest that women who drink more than two cups of drinks with caffeine per day may be more likely to have problems with incontinence.
- Infections of the urinary tract and bladder may cause incontinence for a short time. Bladder control often returns when the infection goes away.
Making the diagnosis
Studies have reported that less than half of women who suffer with UI actually seek help. This is even lower for men. Usually based on symptoms, your doctor is able to make the correct diagnosis. Often, keeping a diary for 2-3 days to track when you empty your bladder or leak urine can show patterns in the incontinence that clarify the possible cause. Sometimes, additional tests, such as urine test, ultrasound or bladder stress test is performed. Less frequently, cystoscopy or urodynamics tests are required for further analysis.
Treatments for Urinary Incontinence
You can take some relatively simple actions at home to help treat urinary incontinence.
Fluid management: Timing food and drink consumption around your activities may help you better control your urge to go. Instead of drinking large amounts of water or other beverages at once, drink smaller amounts at regular intervals throughout the day.
Bladder training: Bladder training requires you to actively delay a trip to the toilet each time you get the urge. You can help control overactive bladder or urge incontinence by going to the bathroom at set times. Start by tracking how often you go to the bathroom each day in a bladder diary. Then slowly add about 15 minutes between bathroom visits. Urinate each time, even if you do not feel the urge to go. By gradually increasing the amount of time between visits, your bladder learns to hold more urine before it signals the need to go again.
Pelvic floor muscle strengthening exercises: These exercises are also known as Kegel exercises. They can help you rebuild strength and tighten muscles in your pelvis and urinary tract system. Ideally, if you are consistent about doing Kegel exercises 3-5 sessions each day, you should see improvement in urinary incontinence within 3-6 months.
Other lifestyle changes may include:
- Lose weight: extra weight puts more pressure on your bladder and nearby muscles which can lead to problems with bladder control.
- Treat constipation: eat foods with lot of fiber, be more physically active.
- Cut back on alcohol, caffeine and carbonated drinks. These substances can stimulate your bladder.
- Stop smoking.
If steps you can take at home do not work to improve your stress incontinence, your doctor may talk to you about these other options:
- Medications:
- After menopause, applying vaginal creams, rings, or patches with estrogen can help strengthen the muscles and tissues in the urethra and vaginal areas.
- For men with enlarged prostates, alpha-blockers like tamsulosin (Flomax) can help with urge or overflow incontinence to more fully empty their bladder.
- For urge incontinence, anti-muscarinic agents and beta-adrenergic agonists help relax the bladder muscle and increase the amount of urine your bladder can hold. Common side effects of anti-muscarinics include tachycardia, edema, confusion, constipation and blurry vision. Adverse effects of beta-adrenergic agonists include GI upset, dizziness, headache and increased blood pressure.
- Botox. Botox injections in the bladder can help if other treatments don’t work for urge incontinence. Botox helps relax the bladder and increases the amount of urine your bladder can hold. Botox effect is temporary and treatments may be repeated every 3-6 months.
- Vaginal pessary. For women, a reusable pessary is a small plastic or silicone device (shaped like a ring or small donut) that you put into your vagina. The pessary pushes up against the wall of the vagina and the urethra to support the pelvic floor muscles and help reduce stress incontinence.
- Bulking agents. The urologist can inject a bulking agent, such as collagen, into tissues around the bladder and urethra to cause them to thicken. This helps keep the bladder opening closed and reduces the amount of urine that can leak out. These injections are temporary and require repeat procedures; frequency depends on agent used.
- Surgery. The two most common types of surgery for urinary incontinence are:
- Sling procedures. The mid-urethral sling is the most common type of surgery to treat stress incontinence. The sling is either a narrow piece of synthetic mesh or a piece of tissue from your own body that your surgeon places under your urethra. The sling acts like a hammock to support the urethra and hold the bladder in place. Serious complications from the sling procedure include pain, infection, pain during sex, and damage to nearby organs, such as the bladder.
- Colposuspension. This surgery also helps hold the bladder in place with stitches on either side of the urethra. This is often referred to as a Burch procedure.
At Inner Vitality in Bellevue, Dr. Alice Kuntz has specifically sought out treatments to help with urinary incontinence that are safe, effective and minimally to non-invasive. We are pleased to offer a variety of treatments to help you gain control over your urine leakage and enhance your quality of life.
- Medical weight loss program to help you shed unwanted fat, especially visceral fat that accumulates in your abdomen, placing more pressure on the bladder and pelvic floor.
- Bioidentical hormone replacement therapy to help balance your hormone levels.
- BTL Emsella™ chair that focuses on strengthening the pelvic floor muscles. Emsella™ has been cleared for treatment of stress urinary incontinence and overactive bladder in women and men. This device is a chair that delivers High-Intensity Focused Electromagnetic technology (HIFEM) to the deep pelvic floor muscles. This energy produces strong pelvic floor muscle contractions, resulting in muscle growth but also is important for re-education and restoration of the neuromuscular control.
- For women, laser vaginal treatment that utilizes gentle laser generated heat to stimulate new blood supply and thicker mucosa in the vaginal wall and thereby help support the bladder and urethra to reduce urinary incontinence.
We welcome you to come in for a comprehensive consultation with Dr. Alice Kuntz. Start your journey to live your best life today.
Drinking Alcohol and Taking Medications
It’s common to experience snoring issues after you drink alcohol or take a sedating medication. Consuming these substances can alter the behavior of the muscles that are located near your airway. When these muscles relax, your airway may become narrower, and your snoring problem could become more severe. For example, you may be more likely to snore if you drink wine or beer before you go to sleep.
Getting Older
As you age, the muscles in your throat may begin to lose strength. These weakened muscles can cause your snoring to become more severe.
Changing Your Sleeping Habits
Your sleeping position can also impact the severity of your snoring problem. In particular, you will be more likely to start snoring if you begin to lie on your back during the night. When you adopt this sleeping habit, gravity will change the position of your tissues, and the width of your airway will decrease. Sleeping on your side may decrease the severity of your snoring.
What Are the Symptoms of a Snoring Issue?
There are a wide variety of physical issues and other symptoms that can be warning signs that you have a snoring problem. Since snoring can be connected with obstructive sleep apnea and other health problems, you should see a medical professional if you are experiencing any of these symptoms.
Developing Nighttime Symptoms
Snoring can cause you to toss and turn while you are sleeping. In addition, you might make rumbling noises, snorts, and other sounds after you fall asleep.
Experiencing Daytime Symptoms
Since snoring will impact the quality of your rest, this problem can cause you to experience symptoms during the day. In particular, you might have headaches in the morning, develop a sore throat, and feel fatigued at your job. Further, you might be unable to concentrate when you are working at your office or spending time with your family.
Damaging Your Partner’s Sleep
If you are in a relationship, your partner may notice the loud sounds that you produce after you fall asleep. As this issue becomes more severe, your partner might wake up during the nighttime. This problem can lead to issues in your relationship and cause your partner to feel tired and unhappy during the daytime.
How Can I Know if I Am Eligible for Treatment?
Before we use our Fotona SP Dynamis laser to address your snoring challenges, we will need to have a customized consultation with you. During this important part of your treatment, we will look at the tissues in your mouth and discuss your health. You should be ready to tell us about the fatigue and other problems that you are experiencing.
You should also tell us if you have used other techniques to address this health condition. After we have reviewed your medical background and symptoms, we will tell you if you are eligible to use this snoring reduction method.
Will the Snoring Reduction Treatment Be Uncomfortable?
Receiving NightLase treatments is a very gentle way to address your snoring problems, and all of your appointments will be comfortable and easy. After you have opened your mouth, we will begin to transmit laser energy into your tissues. Since our Fotona SP Dynamis laser is very advanced, we will be able to widen your airway without harming the other tissues in your mouth.
As we enhance the tissues in your airway, you might experience a gentle tingling feeling or notice a mild increase in temperature. Since these feelings will be very comfortable, you won’t have to use general anesthesia, local anesthesia, or sedating medications during this laser treatment.
How Many Treatment Sessions Will I Need?
The specific length of your snoring reduction plan will depend on the severity of your snoring problem and your response to this laser treatment. In general, you will need to get three treatments at our office in Bellevue. Since we will space out your appointments, your treatment plan may take about 60 days to complete.
Will NightLase Permanently Fix My Snoring Problem?
After you have received three laser treatments, your fatigue and other symptoms may decrease for up to a year. You can extend the benefits of your initial sessions by getting additional laser treatments. For example, you might return to our office for a touch-up treatment after 12 months have passed.
Will I Need To Miss Work To Recover?
If you have a demanding work schedule, you probably won’t want to spend a long time away from your office. Fortunately, you won’t need to avoid your workplace after you receive this laser treatment. Instead, you will typically have a very short recovery period that won’t interfere with your work deadlines, household chores, and other aspects of your schedule.
For example, you might receive this snoring reduction treatment during your lunch break. Once your appointment is finished, you might go back to your workplace and attend meetings, take calls, and complete your other daily tasks. Alternatively, you could go to the grocery store, pick your children up from school, and run other errands.
Improve the Quality of Your Sleep
Experiencing snoring issues can cause you to feel constantly fatigued. Your lack of energy can prevent you from meeting significant deadlines at your job, caring for your family members, and accomplishing other meaningful tasks. Receiving NightLase treatments can be an ideal way to decrease your snoring and other symptoms. To schedule a consultation about this non-invasive treatment, you should contact us at Inner Vitality in Bellevue, WA.